Topography, contour, size and distribution, margins
HSIL lesions are located centrally on the cervix. They are not usually separated from the squamocolumnar junction whether positioned on the ectocervix or within the endocervical canal. The one possible exception is in women who have residual CIN3 lesions following surgery of the cervix. These “skip” lesions may not adjoin the new squamocolumnar junction, but may instead lie proximally within the endocervical canal. When associated with a less severe neoplastic change, CIN3 lesions are generally nearer to the SCJ (figure 11).
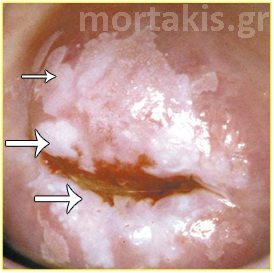
Figure 61 CIN2 lesion of the posterior cervical lip, located centrally in the transformation zone. HSIL are not usually separated from the squamocolumnar junction whether positioned on the ectocervix or within the endocervical canal.
Figure 62 “Skip lesion” located in the endocervical canal, after inadequate CIN3 resection by LEEP.
CIN2 lesions tend to be macular (figure 61), although some are slightly thickened. CIN3 lesions vary from macular to a generalized epithelial thickening that appears as if the intact abnormal epithelium could be peeled away from the underlying stroma. Although a slightly elevated epithelium may be seen, most CIN3 is flat (figures 61, 63).
Figure 63 Small CIN2 lesion at the posterior cervical lip
In general, CIN2 lesions are larger (mean 5,8mm) than CIN1 (mean 4,1mm), but shorter than CIN3 (mean 7,6mm).
CIN3 lesions tend to be confluent, and longer and wider than CIN1 or CIN2 lesions. It is not uncommon to see CIN3 occupy 2 or 3 quadrants of the cervix. Because CIN3 is more confluent and expansive, many lesions will extend into the external os and beyond colposcopic view.
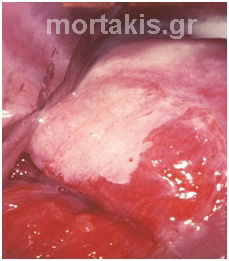
The margins of CIN2 lesions tend to be less irregular or jagged in shape than those in CIN1 lesions. They are generally smooth, rounded, or straight. The apparent external margin may resemble that of CIN1 when a small focal area of CIN2 is positioned within a larger CIN1 lesion (figure 64). CIN2 may also form the peripheral rim around a more centrally positioned CIN3. In this case, the margin is usually fairly straight with only minor variation (figures 65, 66).
Figure 64 The whole transformation zone can be seen. At the top of the picture we see immature squamous metaplasia with mosaic and indistinct borders. Biopsy from a lower position (small arrow) showed CIN1. Biopsies from the squamocolumnar junction (large arrows) showed CIN2.
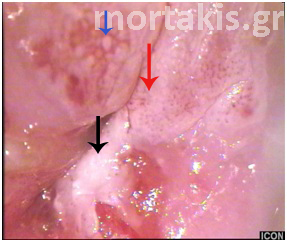
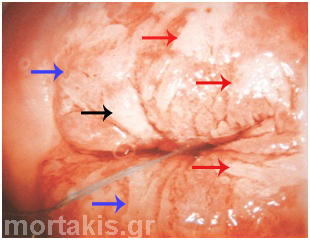
Figure 65 Atypical transformation zone entering the canal. Biopsies from three different positions showed: CIN1 (blue arrow), CIN2 (red arrow) and CIN3 (black arrow). The epithelium of the CIN3 lesion at the posterior lip (cervical os) is thickened. It can be sheared from the underlying stroma because the neoplastic process adversely affects the hemidesmosomes that bind the epithelium to the basement membrane and underlying stroma. A small ulceration can be seen in the area adjoining the avulsed epithelium.
Figure 66 “Lesion within a lesion”. The most serious lesions are located centrally. CIN3 lesion centrally (upper part of the picture –region of cervical os). CIN1 at the periphery. Notice the thick white of the HSIL and the translucent white of LSIL.
The lesion margins of CIN3 are smooth, gently rounded, or straight, creating a distinct demarcation between normal epithelium and neoplastic epithelium. These straight margins are the most common presentation for CIN3 lesions. However, CIN3 may also have peeling edges or internal margins. The thickened epithelium of CIN3 can be sheared from the underlying stroma because the neoplastic process adversely affects the hemidesmosomes that bind the epithelium to the basement membrane and underlying stroma. A small ulceration will usually be seen in the area adjoining the avulsed epithelium (figure 65). To form an internal border, a very large LSIL encompasses a more centrally located CIN3 along the squamocolumnar junction. Colposcopists must remember that the more serious lesions are located centrally (figure 11, 66). CIN3 lesions usually adjoin the new squamocolumnar junction and will enter the canal.
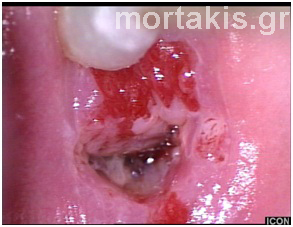
Figure 67 Large CIN3 lesion with distinct margins, occupying the anterior cervical lip. Blood from the os is due to previous Pap smear.
Figure 68 HSIL lesion entering the canal (12 to 1 o’clock). The red areas (major part of the anterior lip and smaller area at 6 o’clock) are due to previous biopsies, which showed CIN3. Final histologic diagnosis, following Leep showed CIN3.
Color
CIN2 lesions are not shiny or snow-white by nature. CIN2 can be described as having an acetowhite color that is generally less translucent than that seen with CIN1 lesions, but less opaque than with CIN3. However CIN2 lesions tend to have an opaque white color derived from greater nuclear density in the epithelium (figure 61). More CIN2 lesions remain acetowhite for a longer time than the more transient acetowhite effect seen with CIN1. Accordingly, the acetowhite color noted in CIN2 is more transient than that seen in CIN3.
Although “dull oyster-grey” and “dense white” have been used to describe the color of CIN3 lesions, it actually may be better to consider the opacity of the epithelium. CIN3 has a nuclear dense epithelium, with abundant protein and little water. As a result, the epithelium functions like a mirror after acetic acid application, reflecting the intense white light of the colposcope back to the colposcopist’s eyes. This opaque white color characterizes CIN3 (figures 9, 10, 11, 40, 41, 65, 67).
CIN3 lesions resemble a wall that has been painted repeatedly with white latex paint. A CIN1 lesion or immature metaplasia more closely resembles a wall that has only received an initial primer coat of white paint or several layers of translucent white watercolor (with the exception of shiny condylomatous lesions)(figures 5, 12, 13, 20, 38, 49, 52, 53, 56, 59). Moreover, the acetowhite effect persists longer in CIN3 lesions than in CIN1 lesions. Therefore, when inspecting a large, complex lesion of the cervix, provided that 5% acetic acid solution was applied uniformly and at the same time to the cervix, the last area remaining acetowhite will likely be the area of most severe disease. (figures 69, 70, 71, 72).
If CIN3 has penetrated the epithelium surrounding and within a gland cleft, then a wide, opaque acetowhite band around a gland opening will be observed (figures 47, 72).
Figure 69 Opaque acetowhiteness of a CIN2 lesion.
Figure 70 CIN2 lesion at the anterior lip of the cervix. Opaque white epithelium. Metaplastic epithelium at the periphery.
Figure 71 Opaque acetowhiteness (oyster white) of a CIN3 lesion
Figure 72 “Dense white” epithelium of a CIN3 lesion above the cervical os. The lesion is well demarcated and its surface is elevated compared with the surrounding normal tissue. The epithelium looks “snow white” but it is not. The problem is that the light of the colposcope is very strong.
Figure 73 CIN2 (red arrows) and CIN3 (black arrow) lesions with opaque acetowhiteness in a large transformation zone. The metaplastic epithelium appears translucent white(blue arrows).
Vessels
Fine to medium caliber vascular patterns of punctation and mosaic can usually be identified in CIN2 lesions. The vessels tend to be of a smaller caliber, more similar to vessels seen in CIN1 than those in CIN3. Occasionally, blood vessels may not be apparent in CIN2, particularly when observed immediately following application of 5% acetic acid solution. However these vessels will become apparent once the acetic acid effect begins to diminish (figure 74).
Coarsely dilated blood vessels, in either punctation or mosaic patterns, are the classic vascular characteristics of a CIN3 lesion. When these coarse vessels are noted, a diagnosis of CIN3 must be considered (figures 17, 21, 22, 23, 24, 75, 76). Furthermore, the intercapillary distances are greater in CIN3 than in CIN1. Vessel patterns and intercapillary distances also tend to be more random, disjointed, and less uniform than in CIN1.
However, it is unusual to see blood vessels in a thick, opaque CIN3 lesion. Physiologically, this can be explained by the fact that expanding blocks of dysplastic epithelium have occluded or pushed aside the afferent and efferent capillary loops normally present. A greater pressure is needed to obstruct the arterial side of the vascular system than the venous system. That may be why in very severe CIN3 lesions, no vessels are noted. With other CIN3, assuming less pressure is exerted by the blocks of neoplastic epithelium; only the venous return is occluded, allowing intense capillary dilatation.
Any evidence of atypical vessels suggests cancer, not CIN3, even though approximately 2% to 6% of histologically confirmed CIN3 lesions demonstrate atypical blood vessels.
Figure 74 Fine to medium caliber mosaic of a CIN2 lesion. Opaque white epithelium, well defined margins.
Figure 75 Coarse punctation and mosaic of a CIN3 lesion. Vessels of large caliber, asymmetry, irregularity. Microinvasion or even invasion cannot be excluded colposcopically in lesions of this type
Figure 76 Coarse punctation and mosaic of a CIN3 lesion of the anterior lip of the cervix above the cervical os. There are also vessel patterns at the lower part of the picture. In this case the enough time has elapsed since the application of acetic acid solution and the area which remained acetowhite longer is seen at 12 o’clock position.
Iodine staining
There is little to no glycogen in the epithelium of CIN2 lesions. Hence, a yellow iodine-negative color will invariably be present following application of Lugol’s solution. There is no glycogen in CIN3 lesions. Hence, a yellow, iodine-negative color appears following application of Lugol’s iodine solution (figure 47). These iodine negative areas match the previously detected acetowhite lesions. Because both CIN2 and CIN3 have iodine negative reaction, Schiller’s test does little to help discriminate CIN2 from CIN3.