Grading systems for colposcopy are systematic methods for predicting colposcopically the severity of lesions by discriminatory analysis of unique colposcopic signs. Aggregate colposcopic signs are more accurately predictive of the clinical severity of cervical disease than individual signs. Attempting to grade lesion severity solely based on the prominence of the acetowhite reaction or by the mere presence of aberrant vessels is unreliable. The colposcopic pictures in figures 91-94 show 3 cases without correlation between impressive colposcopic view and severity of the lesion.
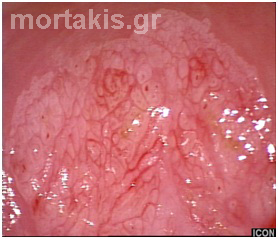
Figure 91 Exophytic condylomata of the uterine cervix. Dense acetowhiteness (though snow-like white), irregular contour without the typical for condylomata micropapillary surface. It would be better to proceed to excision of the transformation zone with a swallow LEEP, in order to have histologic examination.
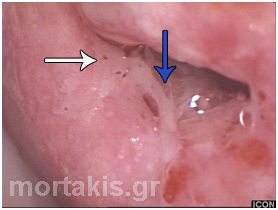
Figure 92 Attempting to grade this lesion’s severity solely based on the mere presence of aberrant vessels is unreliable. Abnormal vascular features such as punctation and mosaics are significant only if these are seen confined to dense acetowhite areas with distinct margins. Histology showed a CIN1 lesion.
Figure 93 Mild acetowhiteness of the lesions shown at the posterior cervical lip (from 3 o’clock to 6 o’clock positions). To the experienced colposcopist, metaplastic epithelium is not organized in an orderly way (see figures 44-46). The end of the atypical metaplastic epithelium towards the canal (new squamocolumnar junction) has well defined margin (blue arrow). There is also an external lesion margin (white arrow). No vascular patterns are present. Histology of the biopsies proved CIN2.
Figure 94 Pregnancy, second trimester. Impressive dense acetowhite exophytic lesions, with irregular surface contour and sharp margins. Multiple biopsies showed CIN2. The lesions disappeared 2 months after delivery.
Several systems exist to help distinguish clinically significant lesions from benign nonneoplastic variants and to grade the severity of lesions. An easy to learn, reproducible system is Reid’s colposcopic index, which assesses margin, color, vascular patterns and iodine uptake.
It must be emphasized that none of the grading schemes is applicable to glandular lesions and grading systems are not applicable to cancer staging.
The importance of a colposcopic grading system was apparent to the inventor of the first colposcope, Dr Hans Hinselmann. He derived a novel, but rather crude, two-part colposcopic grading system which was subdivided into categories of “Simple Atypical Epithelium I and II” and “Highly Atypical Epithelium III and IV”. This early colposcopic grading system became the foundation that other renowned colposcopists modified based on their increased understanding of abnormalities within the transformation zone.
Dr Malcolm Coppleson devised another grading system in the 1960s, focusing attention on color and density of acetowhitening (grade I to III acetowhitening).
In 1976, Dr Adolph Stafl described a system for colposcopic grading based on four factors: surface pattern, color tone, intercapillary distance, and margin contour of the lesion with normal tissue. His grading system was divided into normal, non-significant (inflammation), significant (CIN 1, 2, 3), and highly significant. Much emphasis was placed on the intercapillary distance within lesions, and a method was developed to objectively measure these very small distances. The original work of Kolstad had shown that increased intercapillary distance correlates with more significant histopathologic changes.
Dr Louis Burke further refined the approach to grading cervical lesions. His grading system (grades 1, 2, 3) considered characteristics of lesion surface, margin, color, duration of acetowhite changes and lesion characteristics.
In 1985, Dr Richard Reid described the use of a new and less subjective colposcopic index to differentiate LSIL from HSIL. The Reid’s Colposcopic Index (RCI) considers four colposcopic signs, which are:
- Margin or border of lesion
- Color of lesion following application of 5% acetic acid solution
- Blood vessel characteristics within the lesion and
- Response of the lesion to the application of Lugol’s iodine solution
Each colposcopic sign is subdivided into three categories. Each category is assigned a numerical value from 0 to 2. Each of the four colposcopic signs is considered separately, and numerical scores are assigned respectively, depending on the severity of that characteristic within the detected cervical lesion. The score for each of four colposcopic signs are added to establish a total RCI score. This score is then used to determine the colposcopic impression or estimated severity of the lesions (Table I).
Table I REID’S COLPOSCOPIC INDEX
| COLOSCOPIC SIGN | Zero Points | One Point | Two Points |
| Margin | Condylomatous or micropapillary contour. Indistinct borders. Flocculated or feathered margins. Jagged, angular lesions. Satellite lesions, acetowhite lesions outside the transformation zone | Regular lesions with smooth, straight outlines
Sharp peripheral margins |
Rolled, peeling edgesInternal borders between lesions of different severity |
| Color | Shiny, snow white. Transient, indistinct acetowhite, semi-transparent | Shinny, off-white
Intermediate white |
Dull, oyster grey
Persistent, dense acetowhite |
| Vessels | Fine punctation or fine mosaic. Uniform, fine caliber, nondilated capillary loops | Absence of surface vessels following acetic acid application | Coarse punctation or coarse mosaicIndividual vessels dilatedWide intercapillary distance |
| Iodine Staining | Positive iodine uptake, producing a mahogany brown color.Negative iodine uptake (mustard yellow) of a lesion recognized as low grade by above criteria (1-2) | Partial iodine uptake
Variegated, tortoise-shell appearance |
Negative iodine uptake
(mustard yellow) of a lesion considered high grade by above criteria (3-6) |
| Score | 0-2: Normal or CIN1 | 3-5: CIN1 or CIN2 | 6-8: CIN2 or CIN3 |
The first three colposcopic signs are evaluated following proper application of an acetic acid solution (5%) to the cervix. The score for the final colposcopic sign is dependent on a preliminary subtotal score of the first three signs. The score for the fourth sign can only be determined after application of Lugol’s iodine solution to the cervix.
Grading lesions by assessing the four RCI colposcopic signs
Margins of the lesion
The nature of a lesion margin, edge, or border varies depending on the severity of cervical neoplasia, making it an excellent indicator of the degree of cervical disease. Low-grade lesion (CIN1 or HPV) margins may be irregular, flocculated, feathered, angular or “geographic”, indistinct, exophytic or micropapillary (condyloma-like) in contour or surrounded by small “satellite” lesions. A score of 0 points is assigned to the lesion if these attributes are present (figures 5, 8, 18, 20, 38, 44, 48, 50, 52, 54-59).
In contrast, smooth and fairly straight margins are characteristic of an intermediate lesion (CIN 1, 2). A score of 1 point is assigned to the lesion when these margin characteristics are noted (figures 6, 9, 10, 11, 40, 53, 61, 64, 69, 70, 74, 93).
High-grade lesions, especially CIN3 may have raised, peeling epithelial edges. Distinct lesions encompassed within a larger lower-grade lesion and located closer to the squamocolumnar junction may have an internal border that demarcates the area from the surrounding low-grade change. Lesions with peeling edges or internal margins are likely to be CIN3 and thus receive 2 points for their margin score (figures 11, 41, 66, 67, 95 and 96).
Figure 95 Distinct raised lesion at 1 o’clock position, close to the squamocolumnar junction. Irregular surface contour, dense acetowhiteness. Histology:CIN3.
Figure 96 CIN3 lesion, entering the canal. Raised borders, peeling edges at the posterior cervical lip.
Epithelial color
The color of the lesion following the application of 5% acetic acid solution determines the second colposcopic sign. Low grade (CIN1 or HPV) lesions are semitransparent, nearly translucent or have a shiny snow-white color. These lesions are assigned 0 points for color (figures 6, 7, 8, 18, 20, 38, 39, 48, 51, 53, 59).
CIN3 lesions appear a dirty oyster-gray or very opaque in color after application of 5% acetic acid solution. These lesions appear opaque white because the nuclear dense tissue of the lesion reflects much of the colposcope’s light. They are assigned a score of 2 points for color. The opaque acetowhite color also persists for a longer period of time than does the translucent acetowhite color of CIN1 lesions (figures 9-11, 40, 41, 47, 65-68, 78, 95, 96).
An intermediate (CIN1, 2) lesion is moderately opaque in color, and varies between the 2 extremes of the white color spectrum. This is the most common category for color assignment and it is given a score of 1 point (figures 14, 61-64, 69, 70, 74, 93).
Vascular patterns
The following type of lesions indicates a score of 0: Areas of fine punctation or fine mosaic, ill-defined, yet prominent vessels formed by loose aggregations of nondilated capillaries of uniform caliber. These vessels represent normal intraepithelial looped capillaries that have been exaggerated because of a proliferative effect due to HPV infection (figures 19, 20, 38, 44, 56, 59).
Prominent vascular changes in minor-grade lesions closely resemble the surface vessels seen in congenital metaplasia (figure 92). Hence, it can be quite difficult to distinguish between congenital metaplasia and a low-grade lesion.
The following type of lesions indicates a score of 1: Most CIN2, 3 lesions do not display abnormal surface vascular patterns when dilute acetic acid is applied. Conversely, when the colposcopic examination is performed with saline, these same high-grade lesions have abundant epithelial vessels. This disparity suggests that the application of dilute acetic acid soaking to a high-grade, nuclear-dense lesion causes enough epithelial swelling to transiently compress most intraepithelial looped capillaries, preventing them from being visualized (figures 9, 10, 40, 41, 61, 69, 71-73, 78, 96).
The following type of lesions indicates a score of 2: Coarse, dilated punctation or significant mosaic vascular patterns. These vessels are confined to significant plaques of acetowhite change, dilated, and arranged in sharply demarcated, well-defined patterns (figures 17, 21-24, 74-77, 80, 85, 86).
Iodine staining reaction
The following types of lesions indicate a score of 0: Uniform iodine uptake (positive staining) by intracellular glycogen deposits within well-differentiated epithelium. The chemical reaction between glycogen and iodine produces a deep mahogany-brown color. An area of epithelium that was recognizable as a minor-grade lesion on the three acetic acid criteria (because it scored <3 points) but failed to stain mahogany brown. Histologically, most such lesions represent areas of parakeratosis, without the rich intracellular glycogen stores normally found in benign vaginal mucosa. Despite the absence of intracellular glycogen, the surface keratin deposits in such lesions do retain enough iodine to stain a mustard-yellow color. This pattern is called negative iodine staining (figure 48).
The following type of lesions indicates a score of 1: An irregular mixture of iodine uptake and iodine rejection, imparting a variegated, tortoise-shell appearance. This pattern, termed partial iodine staining is typical of low-grade dysplasia (figure 60).
The following type of lesions indicates a score of 2: Mustard-yellow staining in an area that was already recognized as being high grade by the three dilute acetic acid criteria (figure 47).
It is important to understand that the negative iodine staining seen in both trivial and major lesions is characterized by the same yellow discoloration. Hence, determining whether a focus of negative iodine stain attracts 0 or 2 points depends on the application of other colposcopic features, not on the shade of the iodine reaction.
Accuracy of the Reid Colposcopic Index Grading Scheme
The RCI represents a weighted scoring system that helps colposcopists predict the severity of premalignant cervical lesions. As such, a low RCI score implies less serious cervical disease and a high RCI score indicates more severe disease. Numerator scores from 0 to 2 are predictive of CIN1, HPV-lesions, or normal immature metaplasia. Total RCI scores from 3 to 5 are suggestive of CIN1 or CIN2, with a score of 3 being more predictive of CIN1 and score 5 more suggestive of CIN2. An RCI score from 6 to 8 is predictive of CIN2 to CIN3. An RCI score of 8 is predictive of CIN2 to CIN3. An RCI score of 8 for a cervical lesion demonstrating additional features considered to be warning signs for cervical cancer should be upgraded to a colposcopic impression of either microinvasive or invasive cancer.
The index does not result in scores that are 100% in agreement with histologic findings, but 100% correlation is not the aim. Colposcopic findings that are discordant with histologic findings will occur even when the most experienced colposcopist performs the examination. Nevertheless, use of the index results in more consistent agreement between colposcopic and histologic findings than would be achieved by a less systematic approach to colposcopic diagnosis.