Colposcopy is simply a means of examining the cervix and upper vagina with low-power magnification (x 6-40). Its main use is in the assessment of abnormal cervical cytology, thereby allowing the colposcopist to identify and confirm the extent and characteristics of the abnormal (atypical) epithelium. Colposcopy assists the colposcopist in selecting the most abnormal lesions to biopsy and to rule out the presence of invasive cancer.
The effective management of lower genital tract neoplasia depends on quality colposcopy. Although a final diagnosis is ultimately based on histology, the colposcopist’s presumptive clinical diagnosis is an imperative part of proper evaluation and disease management. Considering cytological, colposcopic and pathologic data we have proper decision making about therapy.
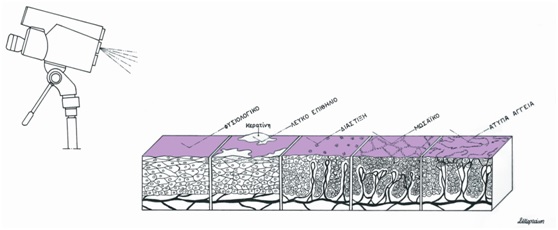
Colposcopy is not a very accurate diagnostic method. The great variability shown in precancerous and cancerous changes is such that no single appearance can be called characteristic. The admixture of the variable blood vessel patterns with varying degrees of epithelial maturity associated with alterations in surface contour, color, and demarcation all determine the great variability in the resulting colposcopic image.
The entire cervical cancer screening can be intended as a risk stratification system, where the results of different exams (cytology, molecular analysis and colposcopy), summed up together determine a risk level which in turn triggers intervention (closer follow up or treatment). In this way the patient is managed by level of risk and not on the basis of histologic diagnosis of a colposcopically directed biopsy.
Using a systematic approach to colposcopic assessment, pioneers of colposcopy such as Burghardt, Coppleson, Kolstadt and Stafl, defined certain colposcopic criteria that were thought to be associated with abnormalities, especially higher-grade lesions. These abnormal findings included: leukoplakia, acetowhite epithelium, surface contour and demarcation of the lesion and vascular pattern (punctation and mosaic patterns, evaluation of intercapillary distance, and presence of atypical vessels). More recently, others have used modifications of these same colposcopic descriptors and have developed grading systems for normal and abnormal findings (Reid, Barbo and Rubin etc)
It is critically important that the colposcopist be able to differentiate among normal, minimally abnormal and significantly abnormal colposcopic patterns.